This eBook from Blue Heron Health NewsBack in the spring of 2008, Christian Goodman put together a group of like-minded people – natural researchers who want to help humanity gain optimum health with the help of cures that nature has provided. He gathered people who already know much about natural medicine and setup blueheronhealthnews.com. Today, Blue Heron Health News provides a variety of remedies for different kinds of illnesses. All of their remedies are natural and safe, so they can be used by anyone regardless of their health condition. Countless articles and eBooks are available on their website from Christian himself and other natural health enthusiasts, such as Julissa Clay , Shelly Manning , Jodi Knapp and Scott Davis. |
How Exercise Programs Reduce Fracture Risk
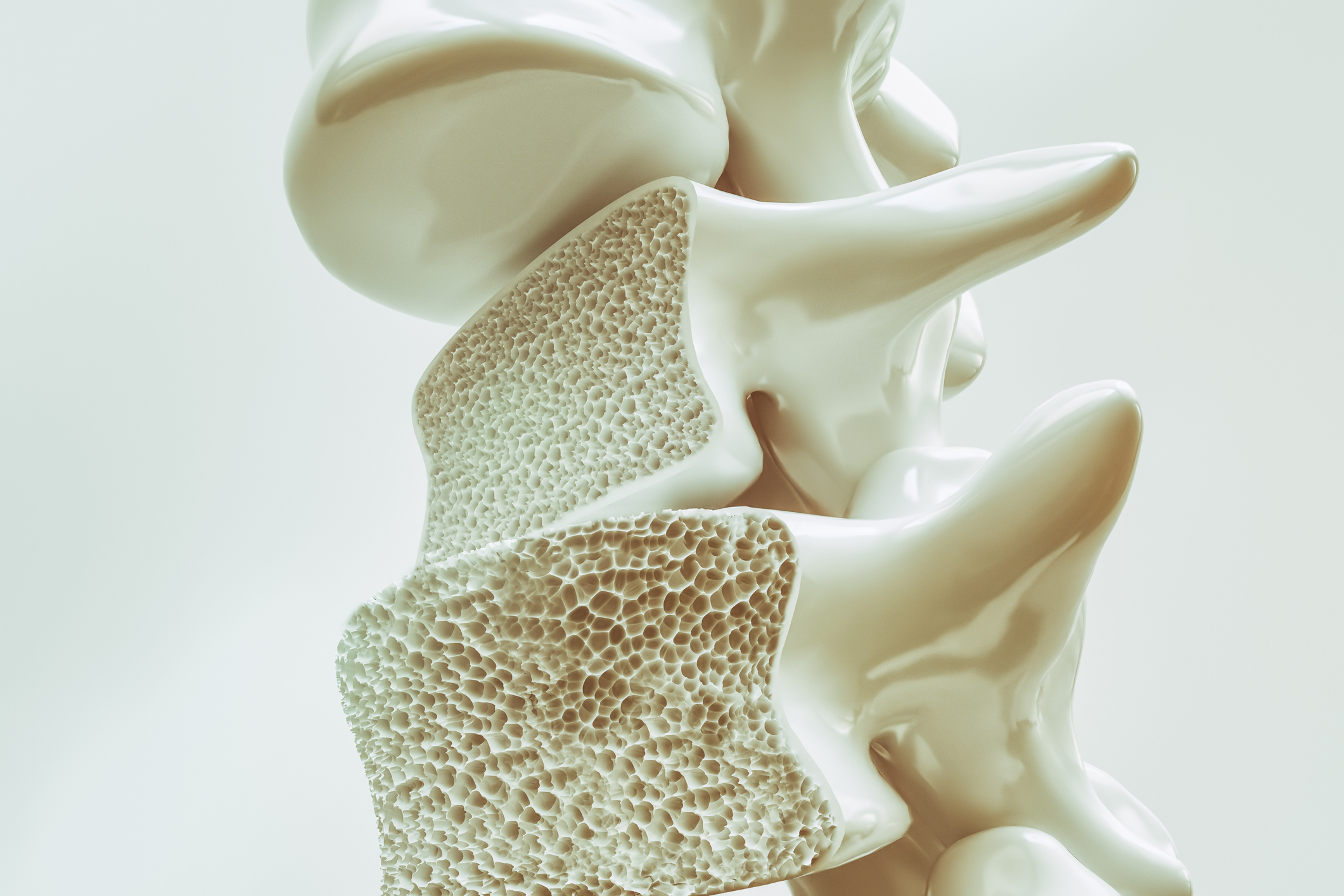
Exercise routines are a significant component of reducing fracture risk, particularly for patients who are at higher risk due to conditions like osteoporosis, age-related bone loss, or low bone density. Physical exercise on a daily basis supports healthier bones, balance, and muscle strength, all of which play a considerable role in reducing fractures. How exercise routines assist in reducing fracture risk is given below:
1. Bone density increase
Weight-bearing exercises (such as walking, jogging, or dancing) induce bone remodeling, where the bone tissue is resorbed and replaced. This enhances bone density or maintains bone strength.
Resistance exercises (such as weightlifting or resistance bands) also build bone density by loading the bones to make them stronger.
Regular physical exercise, particularly weight-bearing and resistance exercises, will slow the bone loss rate and in some cases even enhance BMD to guard against fractures.
Important takeaway: Weight-bearing and resistance exercises activate bone remodeling and help enhance or sustain the density of the bones so that they are less prone to fracture.
2. Enhancing Balance and Coordination
Balance exercises, such as tai chi, yoga, or balance training, improve coordination and reduce the risk of falls. Falls are among the major causes of fractures, especially among the elderly.
Core strength and postural control exercises allow an individual to more easily balance and stand firm, less prone to having falls that lead to fractures.
In addition, the exercises that involve flexibility and joint mobility (e.g., Pilates or yoga) increase overall body awareness that results in balance and reduced injurious falls.
Key takeaway: Balance exercise improves coordination, which reduces fall risk, leading to a subsequent reduction in fractures.
3. Strengthening Muscles
Muscle strength is paramount in the support of bones and the minimization of the stress placed on them during daily function. Natural protection against fractures is achieved through strong muscles by offering stability and absorbing shock in falls or sudden stops.
Resistance training facilitates strengthening of important muscle groups, particularly in the legs, core, and upper limbs, all of which contribute to the prevention of falls and balance maintenance.
As individuals grow older, they lose muscle mass, which can heighten the risk of falls and fractures. Strength training on a regular basis fights this loss of muscle mass, thereby decreasing the risk of fracture.
Key takeaway: Strengthening muscles by resistance training stabilizes bones and decreases the effect of falls, lowering the risk of fractures.
4. Increasing Flexibility
Regular exercise routines that include stretching improves flexibility, thereby improving range of motion and joint health in general. This can help prevent falls caused by restricted movement or incorrect postures.
Stretching exercises can also encourage joint health and mobility, as it is applicable to older adults or those with osteoarthritis or other joint diseases. Proper joint health contributes to the physical stability, hence reducing fracture risk.
Key takeaway: With stretching exercises, flexibility is greater, maintaining mobility and preventing falls.
5. Promoting Healthy Posture
Exercises that correct posture, such as strengthening the core or spine alignment, can decrease the risk of fracture and falls. Correct posture maintains body mechanics and stability, so it is less likely for the individual to lose balance or experience a fall.
Particularly, exercises that enhance the back muscles and preserve good spinal posture have been proven to guard against vertebral fractures, which are common in patients with osteoporosis.
Key point: Exercises that improve posture reduce the likelihood of falls and vertebral fractures since they enhance body stability.
6. Facilitating Joint Health
Low-impact exercises, like swimming or cycling, allow individuals to be active without stressing the bones and joints. These types of exercises are cardiovascular in character but help maintain joint mobility and health.
More movement also triggers synovial fluid production, which lubricates the joints, reducing the risk of stiffness and improving mobility, which helps avoid falls.
Key takeaway: Low-impact activities enhance joint health and mobility, reducing the risk of falls and fractures.
7. Increasing Cardiovascular Health
Cardiovascular exercise (such as swimming, cycling, or brisk walking) increases overall fitness and stamina. Cardiovascular fitness is included in overall physical function, keeping the body strong enough to withstand falls and counter daily activities.
Higher cardiovascular fitness can help older adults or people with chronic disease to preserve strength and energy for safe movement.
Key takeaway: Cardiovascular exercises improve endurance and overall physical fitness, which avoids falls and fractures.
8. Weight Control
Healthy weight is a key component of bone wellness. Being overweight can place undue stress on bones, particularly the weight-bearing joints like the hips, knees, and spine.
Exercise helps control weight, reduce stress on bones and joints, and can also lower the risk of developing a disease like osteoarthritis or joint degeneration that increases the risk of fractures.
Key takeaway: Exercise helps control weight, reduces stress on bones, and lowers fracture risk.
9. Encouraging General Physical Activity
A balanced exercise program involving all types of exercises, such as strength training, aerobic exercise, balance exercises, and flexibility exercises, covers all aspects of bone strength and mobility.
Regular exercise increases bone density, muscle strength, flexibility, and balance, all of which together reduce the risk of falls and fractures.
Key takeaway: A highly balanced, overall exercise program addresses multiple aspects of bone and overall body health, avoiding fractures.
Conclusion:
Exercise is an essential element in the prevention of fractures by increasing bone density, balance, muscle strength, and joint mobility. Incorporating weight-bearing, resistance exercises, balance exercises, and low-impact exercise in the daily plan can significantly limit falls and fractures, particularly for the elderly or individuals with an existing bone concern. A tailored exercise program in its optimal format needs to fit the age, physical condition, and medical situation of an individual to improve best the bones, as well as general health overall, reduce fracture, and augment life quality.
Nutrition therapy plays a crucial part in bone density preservation and fracture risk reduction. Proper nutrition is important to help sustain bone health, especially with aging, when fracture and osteoporosis risks increase. Intake of food with high contents of some nutrients is capable of enhancing bone mineral density (BMD), hence reducing fractures.
Here’s how nutritional interventions and bone density are connected in fracture prevention:
1. Calcium: The Building Block for Bone Health
Calcium is one of the most significant minerals for bone well-being because it is a predominant component of bone tissue. Appropriate calcium intake guarantees bone architecture and strength.
Calcium deficiency leads to bone loss, which can contribute to a higher risk of fractures, especially in older adults and postmenopausal women.
Recommended intake varies by age and sex but is approximately 1,000-1,200 mg per day for most adults. Calcium supplements may be prescribed in those with high fracture risk or low bone density under the supervision of a healthcare provider.
Foods rich in calcium include dairy foods (milk, yogurt, cheese), leafy greens, fortified plant milk, and tofu.
Key point: Bone density and prevention of fractures need sufficient calcium intake, particularly in susceptible populations.
2. Vitamin D: Optimal Calcium Absorption
Vitamin D is critical because it allows the body to absorb calcium efficiently. Without adequate vitamin D, even the best diet rich in calcium will not be an effective bone-builder.
Vitamin D participates in bone remodeling too, aiding the process of bone formation. Deficiency in vitamin D has been associated with higher risk for bone loss, fractures, and osteomalacia (softening of bones).
The adult requirement is approximately 600-800 IU of vitamin D, yet many individuals may require more, especially those who receive little or no sun exposure or some ongoing illness.
Good dietary sources of vitamin D include fatty fish (like salmon, mackerel), egg yolks, and fortified products (like cereals and plant milk). Sunlight is another natural source of vitamin D.
Key takeaway: Vitamin D is required for optimal calcium absorption and bone density to prevent fractures.
3. Protein: Required for Bone Building and Repair
Protein is a health essential nutrient and also has a part in bone repair and formation. The bone tissue has collagen, a protein that provides structural support.
Protein consumption preserves muscle mass, which is necessary for stability and fracture risk reduction, and aids in bone strength. Inadequate protein may impair bone health and increase fracture risk.
The sources of protein include lean meats, fish, poultry, legumes, nuts, and seeds.
The adult daily requirement of protein is approximately 0.8-1.0 g protein per kilogram body weight, although slightly more is needed in the older person or one who has low bone density.
Key point to remember: Protein helps to build bone structure and muscle strength, both of which are necessary to prevent fractures.
4. Magnesium: Assisting Bone Mineralization
Magnesium also plays a crucial role in maintaining bone density, as it is involved in bone mineralization, where calcium is added to the bone matrix.
Magnesium maintains calcium balance and helps in the normal functioning of the bones. Magnesium deficiency leads to bone loss and higher risk of fractures.
Leafy vegetables, nuts, seeds, whole grains, and legumes are magnesium-rich foods.
Important fact: Magnesium plays a critical role in bone mineralization and the maintenance of bone density to reduce the risk of fracture.
5. Vitamin K: Assisting Bone Function and Calcium Management
Vitamin K allows proteins to form which aid in the binding of calcium to the bone matrix, therefore helping to make the bones strong and reducing fracture risk.
Vitamin K also has the function of regulating calcium in the blood so that there is no deposition of calcium in the arteries (and hence no risk of cardiovascular disease).
Food sources of vitamin K include leafy green vegetables (e.g., spinach, kale, broccoli) and fermented foods (e.g., natto, some dairy foods).
Major takeaway: Vitamin K is required for proper calcium regulation and mineralization of bones to reduce the risk of fractures.
6. Boron and Trace Minerals: Bone Health
Boron is a trace mineral that assists in the upkeep of bone health by facilitating the metabolism of calcium and enhancing bone density. It also interacts with magnesium, calcium, and vitamin D to enhance bone health.
Zinc and copper are some significant trace minerals which facilitate bone formation and healing. Their absence may cause damage to bone health.
Boron is found in foods like nuts, apples, grapes, and prunes. Zinc is found in meat, shellfish, and legumes, and copper is found in shellfish, nuts, and seeds.
Key takeaway: Boron, zinc, and copper are adjuncts to maintaining strong bones and preventing fractures.
7. The Role of Antioxidants: Guarding Bone Cells
Antioxidants such as vitamin E and vitamin C protect bone cells from oxidative stress, which will result in the loss of bones and increase fracture risk. Vitamin C is also essential in collagen synthesis, which is a bone structural component.
Citrus fruits, berries, tomatoes, and bell peppers are rich in vitamin C, while vitamin E occurs in nuts, seeds, vegetable oils, and green leafy vegetables.
Key takeaway: Antioxidants protect bone cells from damage and enhance bone integrity for fracture prevention.
8. Phosphorus: Enabling Bone Structure
Phosphorus is a key mineral that plays a role in bone health as part of the structural mineral in bones. It works together with calcium to ensure the protection of bone strength.
While phosphorus is found in a great number of foods (meat, milk, nuts, seeds), excessive phosphorus, particularly when compared to calcium intake, is detrimental to bones. Healthy bones require a good balance of calcium and phosphorus.
Key takeaway: Phosphorus is vital to bone structure but in ratio to calcium consumption for optimal bone health.
9. Hydration: Supporting Joint and Bone Function
Good hydration plays a role in overall health, including joint function. Adequate water intake means the body is able to deliver nutrients, such as for bone function, in an efficient manner and maintain cartilage and joint function.
Water hydration from beverages lubricates the joints, reduces stiffness, and preserves overall mobility, indirectly assisting in fracture prevention by reducing the risk of falls.
Key takeaway: Staying hydrated supports overall bone and joint function, reducing the risk of falls and fractures.
Conclusion:
Nutritional therapy is a component of guaranteeing bone density and reducing the risk of fractures. Crucial nutrients like calcium, vitamin D, protein, magnesium, and vitamin K directly contribute to bone strength, whereas antioxidants and trace minerals act to further protect the bones against degradation. A diet rich in these nutrients, exercise, and a healthy lifestyle can prevent fractures and ensure proper bone health. In those at higher risk of losing bone, for example, the elderly or osteoporotic individuals, special nutritional interventions can be very effective in reducing fracture risk.
The Bone Density Solution by Shelly ManningThe program is all about healthy food and healthy habits. As we discussed earlier, we develop osteoporosis due to low bone density. Therefore, you will have to choose the right food to help your calcium and other vitamin deficiencies. In addition to healthy food, you will have to regularly practice some mild exercises. Your doctor might offer you the same suggestion. However, the difference is that The Bone Density Solution will help you with an in-depth guide.
