This eBook from Blue Heron Health NewsBack in the spring of 2008, Christian Goodman put together a group of like-minded people – natural researchers who want to help humanity gain optimum health with the help of cures that nature has provided. He gathered people who already know much about natural medicine and setup blueheronhealthnews.com. Today, Blue Heron Health News provides a variety of remedies for different kinds of illnesses. All of their remedies are natural and safe, so they can be used by anyone regardless of their health condition. Countless articles and eBooks are available on their website from Christian himself and other natural health enthusiasts, such as Julissa Clay , Shelly Manning , Jodi Knapp and Scott Davis. |
How Cardiovascular Medications Affect Bone Health
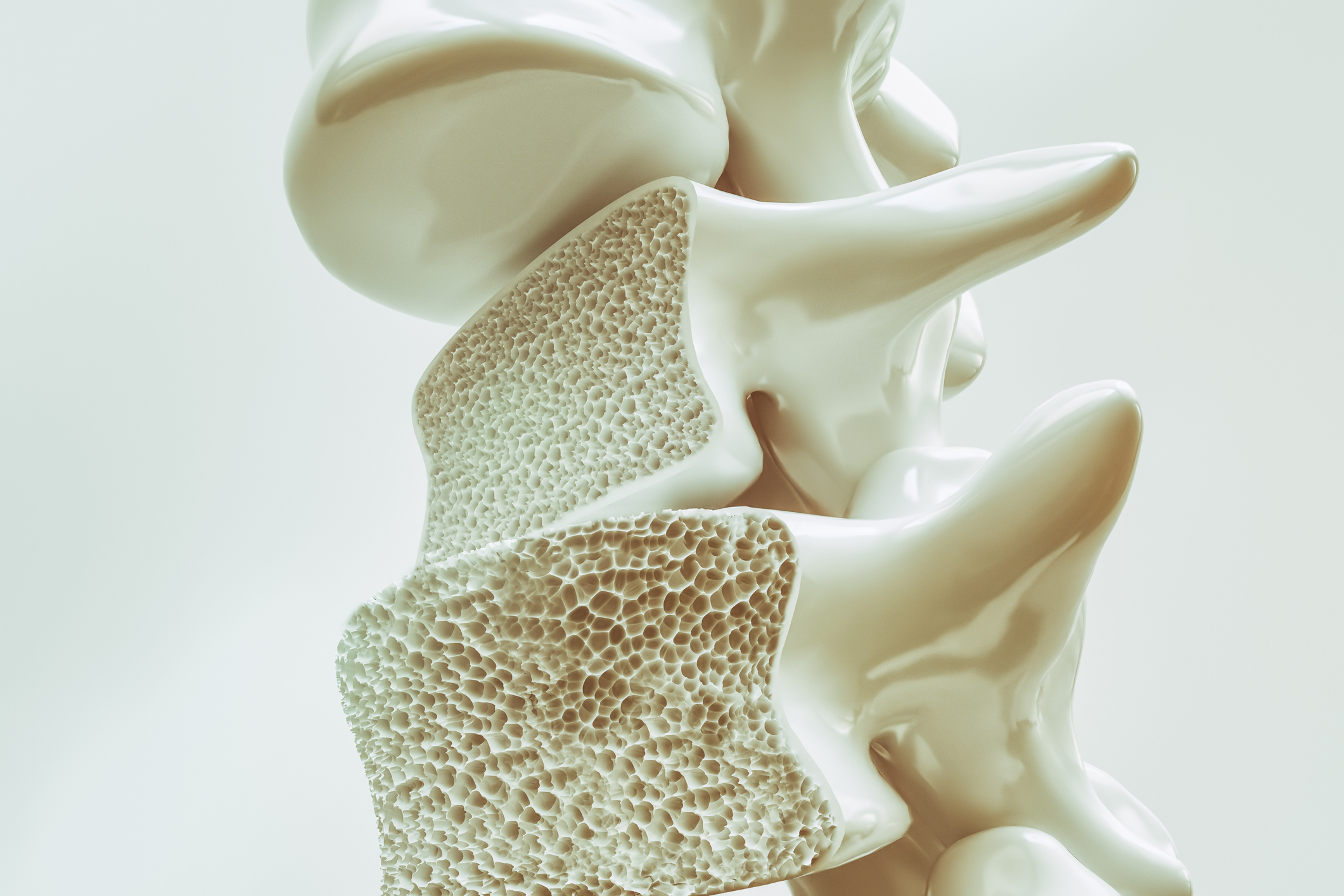
Cardiovascular drugs commonly utilized to manage illnesses like hypertension, heart failure, arrhythmias, and hypercholesterolemia have variable impacts on the health of bones. Certain cardiovascular medications could be adversely affecting bone density, while others are either neutral or even beneficial. Let us dissect the impact of different cardiovascular drugs on bone health:
1. Diuretics
Thiazide Diuretics (e.g., hydrochlorothiazide, chlorthalidone)
Impact on Bone Health: Thiazide diuretics are often used to manage hypertension and heart failure. The medications exert a bone-protective effect by reducing the loss of calcium by the kidneys, which can help maintain or even increase bone density.
Benefit: Thiazide diuretics are also shown to reduce the risk of fractures in some patients. They are particularly useful for patients with osteoporosis or at high risk of bone loss.
Considerations: While thiazides have the effect of improving bone health, they can cause electrolyte imbalances, and hence there is a need for monitoring.
Loop Diuretics (e.g., furosemide, bumetanide)
Impact on Bone Health: Loop diuretics, which are used in heart failure and edema, can potentially increase calcium loss in the urine, leading to higher risk of bone loss and osteoporosis in the long term. This is more relevant with long-term use.
Considerations: Patients on loop diuretics may require supplementation with calcium and vitamin D to maintain bone density, and regular monitoring of their bone density.
2. Beta-Blockers (e.g., atenolol, metoprolol, propranolol)
Impact on Bone Health: Beta-blockers are commonly used to treat hypertension, heart failure, and arrhythmias by reducing blood pressure and heart rate. Overall, beta-blockers have a neutral effect on bone density, i.e., they don’t improve or worsening bone health much.
Studies: Studies have suggested that beta-blockers might even reduce the risk of fractures in elderly patients, maybe because they have the potential to reduce the risk of falls through the control of heart rate and stabilization of blood pressure.
Considerations: Since beta-blockers have minimal effects on bone mineral density, however, long-term effects and general cardiovascular status in the patient must be taken into consideration.
3. Angiotensin-Converting Enzyme (ACE) Inhibitors (e.g., enalapril, lisinopril
Impact on Bone Health: ACE inhibitors are frequently used to treat high blood pressure, heart failure, and chronic kidney disease. These medications have been found to have a mildly protective or neutral effect on bone health. ACE inhibitors may help prevent some degree of bone loss by inhibiting bone resorption (the way in which bones dissolve).
Considerations: ACE inhibitors are not of major impact on bone density, but they can indirectly reduce the risk of fracture by enhancing overall cardiovascular health and reducing the risk of falls.
4. Angiotensin II Receptor Blockers (ARBs) (e.g., losartan, valsartan)
Impact on Bone Health: Like ACE inhibitors, ARBs are used to manage hypertension and heart failure and have been shown to exert a mild protective to no effect on bone mineral density. ARBs block the effect of angiotensin II, which is involved in regulating blood pressure and fluid status. ARBs may prevent bone loss by modulating bone metabolism.
Considerations: ARBs are bone-neutral, i.e., there is no net effect on bone density in either a positive or negative direction.
5. Calcium Channel Blockers (e.g., amlodipine, diltiazem, verapamil)
Impact on Bone Health: Calcium channel blockers are used for the management of hypertension and certain arrhythmias. These medications do not appear to have any significant effect on bone health. They work by preventing calcium from entering cells, leading to relaxation of blood vessels and reduction in blood pressure, but their effect on bone metabolism is minimal.
Considerations: Calcium channel blockers will have no effect on bone density, so they are an attractive option for the hypertensive patient who is susceptible to bone loss.
6. Statins (e.g., atorvastatin, simvastatin, rosuvastatin)
Impact on Bone Health: Statins are primarily prescribed to lower the levels of cholesterol and avoid cardiovascular events. There is some evidence suggesting that statins produce a minor favorable effect on bone health. Statins have the ability to activate the activity of osteoblasts (cells that construct bone) and help in enhanced bone formation.
Studies: Some studies have shown that the use of statins is associated with greater bone mineral density and lower fracture rates in certain populations, but the evidence is not necessarily so.
Considerations: While statins will provide some bone protection, their primary purpose is cardiovascular, and bone health should be monitored independently.
7. Aldosterone Antagonists (e.g., spironolactone, eplerenone)
Impact on Bone Health: Aldosterone antagonists are used to manage diseases like heart failure and high blood pressure. Spironolactone, in particular, leads to bone loss when used for extended periods. This effect is thought to be due to the role aldosterone plays in mineral balance, which indirectly affects bone metabolism.
Considerations: Long-term use of spironolactone may need to be managed cautiously in patients at risk for osteoporosis or fractures. Supplementation with calcium and vitamin D may be necessary, and monitoring of bone density may be warranted.
8. Nitrates (e.g., nitroglycerin, isosorbide dinitrate)
Impact on Bone Health: Nitrates, used in many instances for angina and heart failure, do not directly act upon bone density. They primarily work to dilate blood vessels and boost circulation but have no observable effects upon bone metabolism.
Considerations: Even though nitrates have no direct influence on bone health, their ability to control cardiovascular diseases can potentially contribute towards better overall health and mobility, eventually promoting stronger bones in the long run.
9. Digoxin
Impact on Bone Health: Digoxin is used to treat heart failure as well as specific arrhythmias. Few studies have dealt specifically with its impact on bone health, but it is not thought to have a significant impact on bone density as a whole.
Considerations: As digoxin is primarily prescribed for the treatment of rhythm of the heart and reducing symptoms of heart failure, the effect of digoxin on bone would not be a significant concern, though long-term use needs to be monitored.
10. Anticoagulants (e.g., warfarin, rivaroxaban)
Impact on Bone Health: Anticoagulants are used to prevent blood clots and avoid stroke or heart attack. Warfarin, a vitamin K antagonist, has been known to be linked with reduced bone mineral density and higher fracture rate in some studies. This is because vitamin K is involved in bone mineralization and warfarin affects this process.
Considerations: Warfarin patients should be monitored in terms of bone health, and vitamin K supplementation should be taken into account. Rivaroxaban and apixaban are newer anticoagulants that do not appear to have a similar effect on bone density.
Conclusion
Vascular medications can have similar effects on bone health. Some drugs like thiazide diuretics and statins are bone-protective, while some like loop diuretics and aldosterone antagonists will predispose to bone loss. The severity of the drug effect will vary with most drugs having a neutral effect on the bone. It is essential that patients on cardiovascular medication, especially those with a risk of osteoporosis or fracture, maintain their bone health under control through exercise, appropriate nutrition (calcium and vitamin D), lifestyle modifications, and regular bone density scanning. Management of bone health is an important aspect of the comprehensive care of cardiovascular patients.
Bone density is an intriguing new potential predictor of cardiovascular events, as burgeoning research indicates that low bone mineral density (BMD) is associated with an augmented risk of cardiovascular disease (CVD). It remains unclear why this relationship exists, but research suggests that bone density and cardiovascular well-being have some overlapping etiologic mechanisms. Below is an examination of how bone density can potentially be used to forecast cardiovascular events:
1. Shared Risk Factors Between Osteoporosis and Cardiovascular Disease
Multiple factors lead to both low bone mass and cardiovascular disease:
Age: Both cardiovascular disease and osteoporosis develop with age, particularly in older postmenopausal women and older men. Bone density declines with age, and the tendency to develop atherosclerosis (hardening and stiffening of arteries caused by plaque buildup) is higher.
Inflammation: Chronic inflammation is a key contributor to cardiovascular disease and osteoporosis. Inflammatory markers like C-reactive protein (CRP) are elevated in individuals with cardiovascular disease, and inflammatory markers have also been linked with reduced bone density.
Smoking: Smoking is an established risk factor for both conditions. Smoking can impair blood flow, induce oxidative stress, and accelerate bone loss.
Poor Nutrition: An inadequate diet devoid of essential nutrients, particularly calcium, vitamin D, and potassium, might be the cause of low bone mineral density and poor cardiovascular health.
Physical Inactivity: Physical inactivity may negatively affect both cardiovascular and bone status, such as risk of heart disease and osteoporosis.
2. Bone Mineral Density (BMD) and Cardiovascular Risk
Research has confirmed that reduced bone density may be associated with increased risk of cardiovascular event such as heart attack, stroke, and peripheral artery disease. Reasons behind this correlation are:
Atherosclerosis and Arterial Calcification: The most significant connection between bone health and cardiovascular disease is the process of vascular calcification. This is when calcium deposits form in the lining of blood vessels, most typically in arteries. Although calcium is essential to bone strength, when it deposits in the arteries in error, it can lead to atherosclerosis and enable cardiovascular events.
Contrary to expectations, low BMD subjects have a larger tendency towards vascular calcification. This would mean that the calcium metabolism process not only influences bone health but perhaps also arterial health.
Osteoprotegerin (OPG) and RANKL Pathway: The RANK/RANKL/OPG pathway, which is a major player in bone remodeling, also has a role in the regulation of vascular health. Osteoprotegerin (OPG), a protein that forms bone, may have a potential role in inhibiting vascular calcification and thus reducing cardiovascular disease risk. Dysregulation of this pathway can lead to both lower bone density and increased vascular calcification.
Endothelial Function: Some research shows that patients with lower BMD may have impaired endothelial function (the ability of the blood vessels to dilate and contract normally). Endothelial dysfunction is an important cause of atherosclerosis formation and may be used as a predictor for cardiovascular events.
3. Bone Density and Fractures as Predictors of Cardiovascular Risk
Fracture as a Marker: Fractures, particularly in the elderly, have been associated with increased risk for cardiovascular events. The association may be due to the fact that they have similar risk factors like frailty, low activity, or malnutrition. In others, in those who develop fractures, particularly hip fractures, there may be worsening of cardiovascular health by reduced mobility or secondary events like DVT and PE.
Fracture Risk and Mortality: Studies have shown that individuals who experience fractures due to low bone density may experience higher mortality, and some of the deaths may be due to cardiovascular events. This underlines the importance of monitoring both bone and cardiovascular status in individuals at risk for osteoporosis and fractures.
4. Medications and Their Impact on Both Bone and Cardiovascular Health
Bisphosphonates and Statins: Medications for osteoporosis, such as bisphosphonates, may both positively affect bone health as well as cardiac wellness. Bisphosphonates suppress bone resorption and have been associated with decreased cardiovascular occurrences, particularly among individuals with both heart disease and osteoporosis.
Hormone Replacement Therapy (HRT): In women who are postmenopausal, HRT has been used to manage osteoporosis through the replacement of estrogen. There is evidence that estrogen may be beneficial in its effect on bone density as well as for cardiovascular function by improving lipid profiles and reducing inflammation. The potential risks and benefits of HRT for cardiovascular and bone health need to be individually assessed.
Statins: Statins, also employed to control cholesterol levels and protect against cardiovascular disease, have also been found to have a positive effect on bone health. Certain studies suggest that statins may help prevent bone loss by stimulating the activity of osteoblasts (bone-making cells), but more studies are needed to determine their full effect on bone density.
5. Bone Density Screening as a Predictor for Cardiovascular Risk
Since there are possible connections between cardiovascular events and bone health, interest is growing about whether a bone density test, such as the use of dual-energy x-ray absorptiometry (DEXA) scans, can serve as a cardiovascular risk screening tool. BMD is now used to evaluate osteoporosis and fracture risk but is taken in consideration in the context of its predictive value for cardiovascular events.
Fracture Risk Assessment: It is sometimes used in combination with cardiovascular risk assessment in measures such as FRAX score, which gives an estimate of an individual’s 10-year fracture risk based on a variety of parameters including BMD. The FRAX score considers data such as age, gender, smoking, and prior history of fractures but does not assess cardiovascular risk. However, some research has suggested that fracture-prone patients may also be at greater risk of cardiovascular disease.
Future Research: More studies will be needed to define the function of BMD in predicting cardiovascular risk. Currently, BMD is just one of several considerations in an overall risk assessment, and other factors for cardiovascular risk like cholesterol level, blood pressure, smoking, and family history need to be given equal thought in heart disease prediction.
6. Decreasing Cardiovascular Risk through Controlling Bone Density
Lifestyle Interventions: Healthy lifestyle, i.e., normal exercise (specifically weight-bearing exercises), good diet with proper calcium and vitamin D intake, avoidance of smoking and alcohol, is essential for bone as well as cardiovascular health.
Routine Screening: In those with known cardiovascular risk factors (such as hypertension, diabetes, or high cholesterol), bone density measurement can provide informative data about their condition. Bone density testing along with other cardiovascular risk screening can be recommended by health professionals for those at increased risk of both diseases.
Medication and Treatment: Statins, bisphosphonates, and other bone-protecting medications need to be given serious thought in a patient with cardiovascular disease and osteoporosis. Treatment of either can result in improved health effects and prevention of risk for fracture and cardiovascular disease.
Conclusion
While the path between bone density and cardiovascular risk remains to be explored, evidence does suggest that decreased bone density can be a useful marker of increased cardiovascular risk. Both conditions share common risk factors, such as smoking, inflammation, and diet, and share some of the same biological pathways, such as vascular calcification, that lead to bone disease and cardiovascular disease. Additional research needs to be completed to further characterize the relationship but, with concurrent measurement of bone density along with traditional cardiovascular risk factors, such could allow earlier detection of the at-risk individual for both osteoporosis and cardiovascular events. Treatment of both bone and cardiovascular disease by adjustment of lifestyle and the judicious use of therapy can be applied to mitigate risk in these closely interrelated diseases.
The Bone Density Solution by Shelly ManningThe program is all about healthy food and healthy habits. As we discussed earlier, we develop osteoporosis due to low bone density. Therefore, you will have to choose the right food to help your calcium and other vitamin deficiencies. In addition to healthy food, you will have to regularly practice some mild exercises. Your doctor might offer you the same suggestion. However, the difference is that The Bone Density Solution will help you with an in-depth guide.
