This eBook from Blue Heron Health NewsBack in the spring of 2008, Christian Goodman put together a group of like-minded people – natural researchers who want to help humanity gain optimum health with the help of cures that nature has provided. He gathered people who already know much about natural medicine and setup blueheronhealthnews.com. Today, Blue Heron Health News provides a variety of remedies for different kinds of illnesses. All of their remedies are natural and safe, so they can be used by anyone regardless of their health condition. Countless articles and eBooks are available on their website from Christian himself and other natural health enthusiasts, such as Julissa Clay , Shelly Manning , Jodi Knapp and Scott Davis. |
The Impact of Heart Failure on Bone Density
Heart failure (HF) can have a profound impact on bone density, particularly in individuals with chronic or advanced disease. The relationship between heart failure and bone is complex and multifactorial, influenced both by the disease process and the management of the disease. There are several reasons why patients with heart failure are at increased risk of bone loss and fracture:
1. Chronic Inflammation
Role of Inflammation: Heart failure, particularly chronic heart failure, is associated with systemic inflammation. Inflammatory markers, such as C-reactive protein (CRP), are typically elevated in heart failure patients and can promote bone resorption (destruction of bone tissue). Inflammation can directly affect bone metabolism by enhancing the activity of osteoclasts (cells that resorb bone) and suppressing osteoblast activity (cells that build bone).
Impact on Bone Density: Chronic inflammation also accelerates the loss of bone density, making bones weaker and more susceptible to fractures. This is particularly problematic in older patients with heart failure, who are already at greater risk of osteoporosis.
2. Reduced Physical Activity
Impaired Mobility: Patients who have heart failure often experience symptoms such as shortness of breath, fatigue, and weakness that can severely limit their degree of physical activity. Physical inactivity is one of the main risk factors for osteoporosis and bone loss because weight-bearing activity, such as walking or resistance exercise, is important in maintaining bone density.
Muscle Weakness: Physical inactivity results in muscle wasting and weakness, which not only causes poor physical function but also affects bone health. Healthy muscles support bone health by putting forces on bones with each movement, stimulating the formation of bone.
3. Medications Used in Heart Failure
Diuretics: Diuretics, which are used in the management of heart failure to reduce fluid overload, affect bone health by increasing the excretion of calcium through the kidneys. The loss of calcium can result in decreased bone density over time, particularly if dietary intake of calcium and vitamin D is low.
Loop Diuretics: More potent diuretics like furosemide can cause an even greater impact on calcium loss and decreased bone density, placing one at risk of osteoporosis.
ACE Inhibitors and ARBs: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), which are standard therapy for patients with heart failure, have a neutral or slightly protective effect on bone. They do not, however, effectively antagonize the osteoporosis of heart failure.
Beta-Blockers: These medications, which are used to manage symptoms of heart failure and reduce cardiac workload, also appear to have a neutral effect on bone density. There is no strong evidence that beta-blockers improve or harm bone health.
Aldosterone Antagonists: Medications such as spironolactone, which are used in the management of heart failure, can reduce water retention and have been linked to lower bone mineral density in some studies. However, their effect on bone health is still uncertain, and more research is needed in this area.
4. Hormonal Changes
Effect on Sex Hormones: Heart failure, especially in older adults, can influence the production of hormones such as estrogen and testosterone, both of which play a role in maintaining bone density. In women, low estrogen levels (due to menopause or heart failure-induced hormonal changes) predispose them to osteoporosis. In men, low testosterone levels can also cause bone loss.
Renin-Angiotensin System: The renin-angiotensin system, which regulates blood pressure and fluid balance, is typically dysregulated in heart failure. This system has an indirect influence on bone metabolism, affecting both bone formation and bone resorption, with the potential to lead to excessive bone loss.
5. Nutritional Deficiencies
Calcium and Vitamin D Deficiency: Patients with heart failure are at greater risk of malnutrition, and some also have a low diet in the way of basic nutrients such as calcium and vitamin D. Both of these nutrients have important roles to play in bone health. A lack of calcium and vitamin D can exacerbate bone loss and fracture risk.
Malabsorption: Gastrointestinal symptoms such as bloating, nausea, and vomiting in advanced heart failure can lead to malabsorption of nutrients, further increasing the risk of bone disease.
6. Impaired Kidney Function
Kidney Disease and Bone Health: Chronic kidney disease (CKD) often occurs together with heart failure and can also affect bone density. The kidneys play a role in the regulation of calcium and phosphate levels, and compromised kidney function can lead to imbalances that trigger bone breakdown and inhibit bone formation. In addition, diuretic medications used in the management of heart failure can further compromise kidney function and exacerbate bone loss.
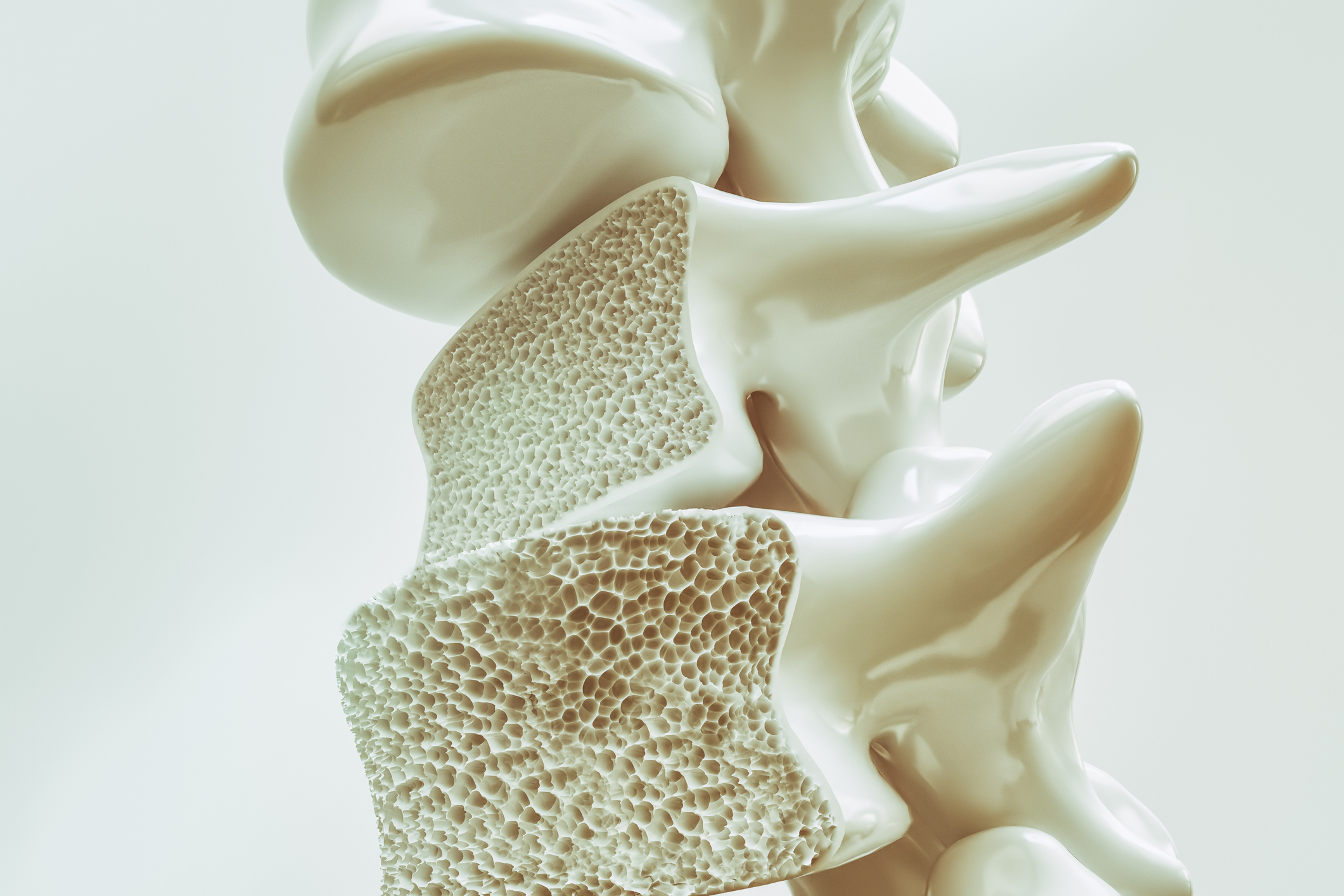
7. Osteoporosis and Fracture Risk
Increased Fracture Risk: The combined effect of inflammation, lack of physical activity, medication side effects, and nutritional deficiencies in heart failure patients significantly increases fracture risk. Hip, spine, and falls-related fractures are of great concern as they tend to worsen the overall health and quality of life in patients with heart failure.
Clinical Outcomes: Patients with heart failure who experience fractures are likely to experience longer lengths of stay, poorer functional outcomes, and higher mortality. Osteoporosis and bone loss worsen the management of heart failure and also complicate the recovery from acute events.
8. Management of Bone Health in Heart Failure
Bone Density Screening: Patients with heart failure, especially those who are at risk due to age, immobility, or use of medications that affect bone density, need to have regular screening for osteoporosis or screening for low bone mineral density (via a DEXA scan).
Calcium and Vitamin D Supplements: Having enough calcium and vitamin D is crucial for bone health. Supplements may be prescribed for patients with heart failure who are at risk of deficiency.
Physical Activity: Even in heart failure patients, supervised physical activity is necessary to maintain bone density and increase muscle strength. Weight-bearing, low-impact exercises such as walking or low resistance training can stimulate bone growth and improve physical function overall.
Osteoporosis Medications: Certain medications can be administered to some patients with heart failure and osteoporosis solely for the health of bones, such as bisphosphonates or denosumab, to prevent bone loss and reduce the risk of fracture.
Dietary Changes: A diet rich in nutrients with foods known to enhance bone health, including calcium, vitamin D, protein, and other minerals, is essential. A balanced diet can even reverse some of the negative effects of heart failure on bone density.
Conclusion
Heart failure has a considerable impact on bone density due to multiple mechanisms, including chronic inflammation, reduced physical activity, medications, endocrine changes, and nutritional deficiencies. Patients with heart failure are also at greater risk of osteoporosis and fractures, which can further worsen overall health status. Keeping a watch on bone health on a regular basis, maintaining proper nutrition, exercise, and appropriate changes in medications are all significant in minimizing the risk of bone loss and fractures in heart failure patients. Bone health management in heart failure patients is an essential aspect of comprehensive care to improve quality of life and long-term clinical outcomes.
Bone density and cardiovascular risk factors are interconnected because many of the same drugs, diseases, and lifestyle behaviors that impact cardiovascular health also influence bone health. Both bone density and cardiovascular health are important components of overall health, particularly as age advances. The following is a review of the impact of cardiovascular risk factors on bone density and the risk of osteoporosis:
1. The Interconnection Between Cardiovascular Disease and Bone Health
Shared Risk Factors: Osteoporosis and CVD have several shared risk factors, including poor diet, physical inactivity, smoking, and excessive alcohol consumption. These risk factors are detrimental to both the cardiovascular system and the bones.
Smoking: Smoking has been demonstrated to contribute to the development of both cardiovascular disease and low bone density. It impedes blood supply, reducing the amount of nutrients reaching bones, and provokes the activity of bone-resorbing cells (osteoclasts), which increases bone loss.
Alcohol Consumption: Excessive alcohol intake can interfere with bone formation and increase the risk of fractures. It also increases blood pressure and the risk of heart disease.
Unhealthy Diet: An unhealthy diet lacking calcium, vitamin D, and other nutrients essential for bone strength (like magnesium and potassium) can weaken bones and cause osteoporosis. Meanwhile, a diet high in saturated fat can cause high cholesterol levels and set one up for heart disease.
Physical Inactivity: Inactivity can weaken bones and make osteoporosis more likely. Exercise also decreases blood pressure and enhances cardiovascular function.
2. Hypertension and Bone Health
Impact of High Blood Pressure (Hypertension): Hypertension, or high blood pressure, is a major risk factor for cardiovascular disease and also has been linked to low bone density. Chronic high blood pressure can lead to increased inflammation in the body, which might stimulate bone-resorbing cells (osteoclasts) and increase bone loss.
Medication Effects: Some medications used to treat hypertension, such as diuretics, beta-blockers, and calcium channel blockers, have side effects that can affect bone health. For example:
Diuretics: These medications can lead to the loss of calcium and other minerals from the body that are essential for bone health, which increases the likelihood of bone density loss.
Beta-blockers and Calcium Channel Blockers: There is some evidence to suggest that certain medications for blood pressure can disturb bone remodeling by disrupting the equilibrium between bone resorption and bone formation, leading to a reduction in bone density over time.
Management of Hypertension: Treatment of high blood pressure through lifestyle modification (i.e., diet, exercise, stress management) and medications without negative impact on bone health is essential to reduce both cardiovascular risk and osteoporosis risk.
3. Cholesterol and Bone Density
High Cholesterol and Bone Health: Elevated levels of cholesterol, particularly low-density lipoprotein (LDL) cholesterol (so-called “bad” cholesterol), have been linked to lower bone density. This may be due to the fact that the inflammatory process of high cholesterol can activate the function of osteoclasts (bone-resorbing cells) and lead to bone loss.
Statins and Bone Health: Statins, commonly prescribed to lower cholesterol levels, have been examined for their potential influence on bone density. Some research suggests that statins have a positive effect on bone health by stimulating osteoblasts (bone-forming cells) and suppressing bone resorption. However, the evidence is inconclusive, and more studies are needed to establish the long-term effect of statins on bone health.
4. Diabetes and Bone Density
Type 1 and Type 2 Diabetes: Both type 1 and type 2 diabetes have been associated with an increased risk of low bone density and osteoporosis. Diabetes affects bone health in several ways:
Hyperglycemia: Chronic high blood sugar can lead to the formation of advanced glycation end products (AGEs), which damage collagen in the bone matrix, causing bones to become weaker.
Insulin Resistance: Type 2 diabetes insulin resistance can interfere with the normal process of bone cells, reducing the ability of osteoblasts to form new bone.
Risk of Fractures: Diabetic individuals are at higher risk for fractures even when bone density levels appear to be within the normal. This may be due to changes in bone quality, including the composition and strength of the bone tissue.
Diabetes Management: Diabetic patients require strict blood glucose control and regular monitoring of their bone density to reduce bone loss and fractures. Certain medications, such as bisphosphonates (drugs used for osteoporosis treatment), may be given in some cases for the protection of bones.
5. Obesity and Bone Density
Impact of Obesity: Obesity is a risk factor for both cardiovascular disease and poor bone health. While excessive body weight can lead to greater bone density due to the heightened load on bones, obesity can also negatively impact bone health in the following manner:
Inflammation: Obesity is associated with chronic low-grade inflammation, which can stimulate osteoclast activity and lead to bone resorption.
Endocrine Changes: Obesity can lead to changes in hormone levels, such as hyperleptinemia and reduced levels of adiponectin, both of which have negative impacts on bone.
Visceral Fat: Fat stored around internal organs, or visceral fat, has also been linked to higher levels of inflammatory markers and reduced ability to maintain healthy bone density. Additionally, excess body weight can increase mechanical stress on bones, perhaps accelerating the deterioration of joint cartilage and increasing fracture risk.
6. The Role of Inflammation in Cardiovascular Risk and Bone Density
Chronic Inflammation: Both cardiovascular disease and low bone density are also associated with chronic inflammation. Inflammation promotes the production of cytokines (inflammatory molecules) that possess the capacity to stimulate osteoclast activity, leading to increased bone resorption and decreased bone density.
Systemic Inflammation and Osteoporosis: Individuals with cardiovascular conditions such as atherosclerosis, heart failure, or stroke also have elevated systemic inflammation, which has a detrimental impact on bone metabolism and increases the risk for osteoporosis and fractures.
7. Cardiovascular Disease Medications and Bone Health
Corticosteroids: Corticosteroids are prescribed to treat a variety of diseases, including heart disease, but long-term therapy can lead to bone loss and osteoporosis. Corticosteroids can inhibit bone formation and activate the bone-destroying cells (osteoclasts), thus leading to reduced bone density.
Other Medications: Some drugs that are prescribed for treating heart failure, high blood pressure, and high cholesterol also impact bone density. Bone health needs to be checked regularly in individuals taking these medications, particularly with prolonged use.
8. Managing Cardiovascular Risk Factors to Protect Bone Health
Balanced Diet: A diet rich in calcium, vitamin D, and other bone-enriching nutrients that also consists of heart-healthy foods like fruits, vegetables, whole grains, and lean proteins can improve both cardiovascular and bone health.
Physical Activity: Regular weight-bearing exercise like walking, running, or resistance training can improve bone density and cardiovascular health. Exercise also helps with weight control, blood pressure regulation, and reduction of inflammation.
Medications and Supplementation: Medications to manage blood pressure, cholesterol, and diabetes should be carefully chosen to prevent adverse effects on bone health. Calcium and vitamin D supplementation can also be administered for individuals at risk of osteoporosis.
Weight Control: Maintaining a healthy weight by diet and exercise can reduce the risk of both cardiovascular disease and osteoporosis. Preventing excess weight gain, particularly around the waistline, can also avoid inflammation that is unhelpful to bone health.
Conclusion
Cardiovascular risk factors of hypertension, high cholesterol, diabetes, and obesity all affect bone health in some fashion. Chronic inflammation, endocrine alterations, and the use of certain medications can cause bone density loss, increasing vulnerability to osteoporosis and fractures. Management of such cardiovascular risk factors through lifestyle intervention, medication, and surveillance is important for maintaining both cardiac and skeletal health. A combined approach with a well-balanced diet, regular physical activity, and good medical care can weaken the effects of cardiovascular risk factors on bone density, maintaining general well-being and minimizing fractures and cardiovascular incidents.
The Bone Density Solution by Shelly ManningThe program is all about healthy food and healthy habits. As we discussed earlier, we develop osteoporosis due to low bone density. Therefore, you will have to choose the right food to help your calcium and other vitamin deficiencies. In addition to healthy food, you will have to regularly practice some mild exercises. Your doctor might offer you the same suggestion. However, the difference is that The Bone Density Solution will help you with an in-depth guide.
