This eBook from Blue Heron Health NewsBack in the spring of 2008, Christian Goodman put together a group of like-minded people – natural researchers who want to help humanity gain optimum health with the help of cures that nature has provided. He gathered people who already know much about natural medicine and setup blueheronhealthnews.com. Today, Blue Heron Health News provides a variety of remedies for different kinds of illnesses. All of their remedies are natural and safe, so they can be used by anyone regardless of their health condition. Countless articles and eBooks are available on their website from Christian himself and other natural health enthusiasts, such as Julissa Clay , Shelly Manning , Jodi Knapp and Scott Davis. |
The Influence of Bone Density on Vascular Health
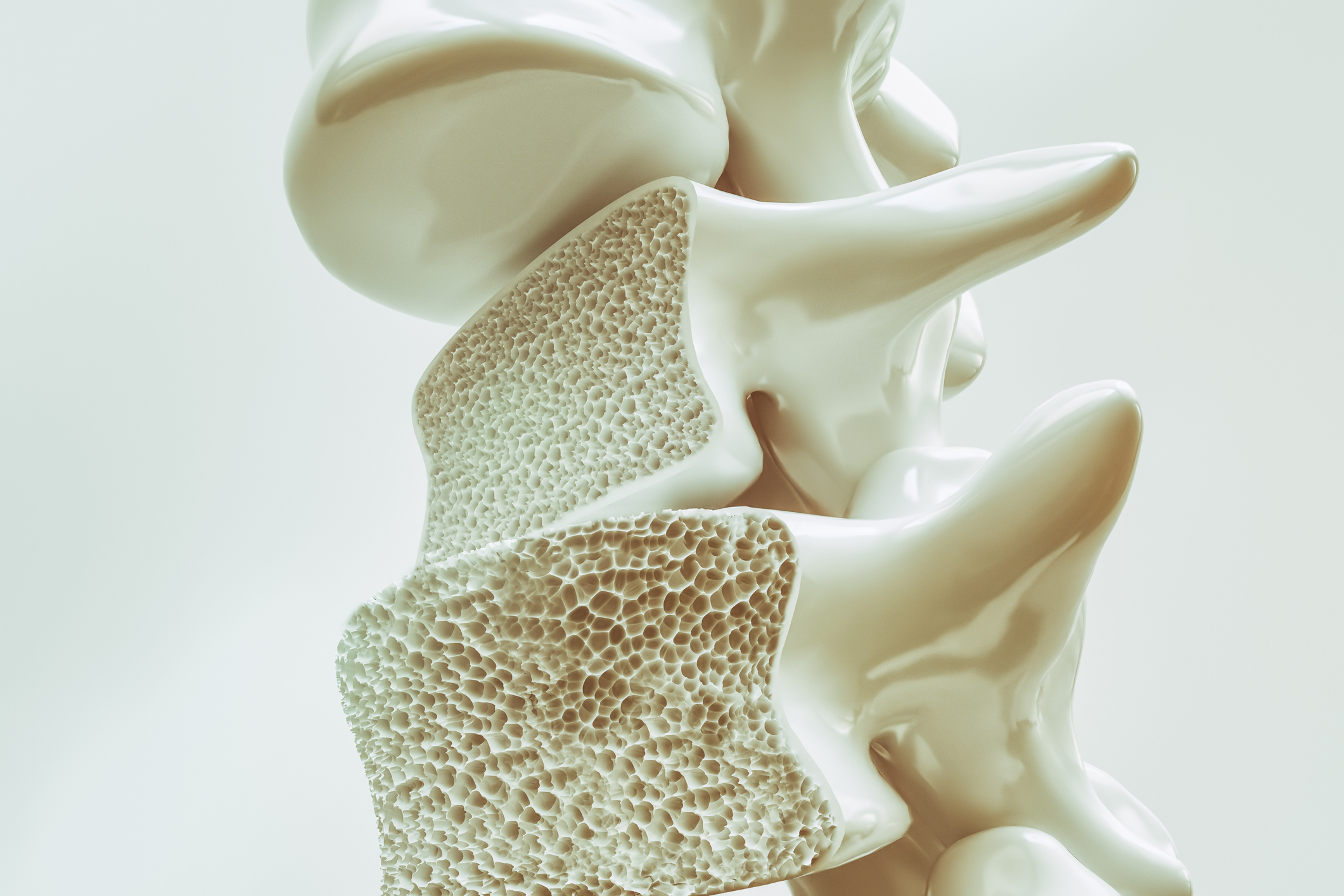
The interface between bone density and vascular health is a new area of research, with increasing evidence that changes in bone status may affect blood vessel and cardiovascular function. While bones and blood vessels are part of different organ systems, they share common mechanisms for mineral homeostasis and inflammation. The following is an overview of the ways in which bone density may affect vascular health:
1. Shared Pathophysiological Mechanisms
Bone and vascular tissues are both dependent upon mineral regulation of such minerals as calcium and phosphate, and their dysregulation can affect the two systems.
Calcium Metabolism: Vascular health and bone density both come to be impacted by calcium regulation. Bone formation is dependent on calcium but with disorder of the calcium metabolism, deposition of calcium takes place within the walls of blood vessels resulting in hardening of vessel walls.
Bone Resorption and Vascular Calcification: Bone resorption (destruction of bone tissue) occurs in osteoporosis because of an imbalance between bone formation and resorption. Similarly, in blood vessels, some proteins related to bone metabolism, osteoprotegerin (OPG) and RANKL (receptor activator of nuclear factor-kappa B ligand), are possibly involved in arterial calcification. This can lead to atherosclerosis and enhanced cardiovascular risk.
2. Vascular Calcification and Bone Density
Vascular Calcification: This is a disease process where calcium and phosphate deposits accumulate in the blood vessels. It may be in arteries or veins and is often seen in people with atherosclerosis, kidney disease, or diabetes. Vascular calcification hardens blood vessels, elevating blood pressure and leading to heart disease by preventing the expansion and contraction of blood vessels with blood.
Bone Mineral Density and Arterial Calcification: There has been a theory of a “bone-vascular axis,” whereby diminished bone mineral density (osteoporosis) is correlated with a higher risk of vascular calcification. Conversely, augmented bone mineral density is correlated with diminished vascular calcification, and thus potentially there is a protective association between bone and vascular health. This is thought to be due to shared mechanisms of inflammation and mineral control that affect both vascular and bone tissues.
3. Inflammation as a Common Link
Chronic Inflammation: Vascular disease and reduced bone density are both associated with chronic low-grade inflammation. Inflammatory markers, such as C-reactive protein (CRP), are elevated in osteoporotic and atherosclerotic patients, suggesting that systemic inflammation may play a role in the pathogenesis of both conditions.
Pro-inflammatory Cytokines: Pro-inflammatory cytokines like TNF-alpha and IL-6, which have increased levels, have been found to be implicated both in vascular calcification and bone resorption. These cytokines have the potential to stimulate osteoclast activity (cells which break down bone tissue) and are implicated in the mechanisms leading to the hardening of arteries, thereby linking bone density and cardiovascular health.
4. Osteoporosis and Cardiovascular Disease
Shared Risk Factors: Both osteoporosis and cardiovascular disease have shared risk factors, such as aging, smoking, inactivity, and poor diet. These risk factors can increase both the risk of low bone density and vascular damage. For instance, physical inactivity results in weakened bones and also in the formation of arterial plaque, which can increase the risk of heart disease.
5. Hormonal Changes: Hormonal declines, particularly a decrease in estrogen level at menopause, may cause bone loss as well as cardiovascular risk. Estrogen has been noted to be protective on bones and on arterial walls, so a decrease in estrogen will directly lead to osteoporosis and atherosclerosis.
5. Bone-Specific Factors Affecting Vascular Health
Osteoprotegerin (OPG) and RANKL: OPG and RANKL are regulators of bone remodeling and have been found to also affect vascular health. OPG is a protein that acts to inhibit osteoclasts, which stop excessive bone breakdown, but seems to also act to inhibit vascular calcification. RANKL, which acts to stimulate osteoclasts, is implicated in vascular calcification as well. The relative balance between OPG and RANKL has been considered important in the regulation of both bone density and vascular calcification.
Matrix Gla-Protein (MGP): MGP is an important inhibitor of vascular calcification. It prevents calcium deposition in blood vessels, and vitamin K controls its activity. Decreased bone mineral density is usually associated with diminished MGP activity, which may proceed to encourage increased vascular calcification and arterial stiffening.
6. The Impact of Bone Health on Cardiovascular Risk:
Bone Density as a Cardiovascular Risk Predictor: Low bone density has been shown by recent studies to be a predictor of increased cardiovascular risk. Low bone mineral density or osteoporosis in certain studies has been shown to be at increased risk of developing cardiovascular conditions like coronary artery disease, stroke, and heart failure. This is said to be due to shared risk factors and mechanisms that influence bone as well as vascular health.
Intervention Implications: As a result of the interdependence between bone density and vascular health, interventions aimed at improving bone health can also benefit cardiovascular health. For example, medications to increase bone density, such as bisphosphonates or denosumab, can inhibit vascular calcification. Exercise, proper diet, and quitting smoking can help bones and blood vessels and perhaps reduce the risk of both osteoporosis and cardiovascular disease.
7. Clinical Implications
Comprehensive Health Approach: Providers need to consider both bone health and cardiovascular health in patients, especially older or at-risk patients for either or both disease states. Patients with osteoporosis, for example, should be assessed for cardiovascular risk factors, and patients with atherosclerosis should be assessed for bone density. Treating both disease states simultaneously demands consideration of shared risk factors, such as diet and exercise.
Monitoring and Early Intervention: Detection of early vascular calcification by imaging (e.g., CT scans or ultrasound) and monitoring of bone density by dual-energy X-ray absorptiometry (DEXA) scan will enable individuals at risk for both conditions to be detected. Early intervention with lifestyle modification, drugs, and follow-up can reduce the burden of osteoporosis as well as cardiovascular disease.
Conclusion
Bone density and vascular health are closely related by shared mechanisms of mineral metabolism, inflammation, and hormonal regulation. Low bone density is associated with increased risk of vascular calcification and atherosclerosis, while improved bone health has the potential to prevent vascular injury. This association can be applied to inform prevention and treatment of osteoporosis and cardiovascular disease. A general approach of health, with regard to diet, exercise, and early treatment, is needed to improve results for individuals at risk for both diseases.
Bone density and cardiometabolic health are closely linked, with blood pressure, cholesterol, glucose metabolism, and inflammation influencing bone as well as cardiovascular health. Bone density and cardiometabolic health are dependent on each other, with each system sharing common risk factors and mechanisms. Unveiling this relationship can make it easier to design strategies for osteoporosis and cardiovascular disease (CVD) prevention, especially in elderly individuals.
1. Bone Density and Cardiometabolic Health: A Relationship
Bone density is defined by the amount of minerals (primarily calcium) in the bone tissue, which affects bone strength and resistance. On the other hand, cardiometabolic health is a combination of cardiovascular health and metabolic health including blood pressure, cholesterol level, blood sugar level, and body fat patterning.
The following are some of the most significant ways in which cardiometabolic health influences bone density:
2. Influence of Obesity on Bone Density
Obesity is associated with an increased risk of low bone density and osteoporosis despite increased weight and mechanical loading on the bones. This is primarily due to adiposity (fat accumulation), leading to chronic low-grade inflammation, which alters bone metabolism.
Visceral fat, or fat that surrounds internal organs, has proven to be most harmful to bone. It releases inflammatory cytokines (such as interleukin-6), which inhibit osteoblast function (bone-building cells) and enhance osteoclast activity (bone-releasing cells), leading to loss of bone.
Additionally, obesity-related insulin resistance and hyperinsulinemia (elevated blood levels of insulin) can disrupt bone remodeling, resulting in a mismatch between bone resorption and formation, which eventually may reduce bone mineral density (BMD).
3. The Role of Diabetes in Bone Health
Type 2 diabetes is a significant risk factor for low bone density and fractures. The association is best explained by several interacting mechanisms:
Hyperglycemia and insulin resistance may perturb bone metabolism, disrupting osteoblast function and increasing osteoclast activity, leading to bone resorption.
Chronic hyperglycemia can lead to advanced glycation end products (AGEs), which deposit in bone and are detrimental to bone mineralization and strength.
Diabetic medications, such as thiazolidinediones (used to treat insulin resistance), can lead to bone loss through the promotion of osteoclast activity.
Type 1 diabetes, while less common, also causes bone issues because of uncontrolled glucose and insulin or insulin-like growth factor (IGF-1) deficiencies, both of which play a role in bone formation.
4. Bone Health and Hypertension (High Blood Pressure)
Hypertension is one of the key risk factors for cardiovascular disease and bone loss. Uncontrolled high blood pressure can affect bone health in a number of ways:
Renal impairment: Chronic hypertension may lead to kidney damage, interfering with calcium metabolism and leading to low calcium reserves in the bones and subsequently bone loss.
Medications: Some antihypertensive drugs, such as loop diuretics, may lead to urinary loss of calcium, leading to bone weakening in the long term.
Increased oxidative stress that is associated with high blood pressure may lead to cell damage that produces bone-forming cells and induce osteoclast activity, leading to bone resorption.
On the other hand, blood pressure control by altering lifestyle or medication with ACE inhibitors or calcium channel blockers can help bone health by improving vascular health and reducing inflammation.
5. Cholesterol and Bone Density
Cholesterol plays a multi-faceted role in bone. While high LDL cholesterol is associated with cardiovascular disease, its relationship with bone mineral density is not yet well understood. Some studies suggest that high LDL cholesterol can lead to low bone density, likely due to its effect on inflammation and vascular health.
Hypercholesterolemia potentially can lead to the deposition of oxidized LDL, which elevates oxidative stress and bone cell injury. Increased cholesterol also is linked with arterial stiffness and compromised blood flow, which can lower nutrient delivery to bone tissue.
Statins, the medication, which is consumed to lower cholesterol, may be beneficial for people’s bones by lowering inflammation and improving bone remodeling, albeit with potential conflicting data. There are some studies, which include that statins can promote the growth of bone, while others suggest that they have no direct effect on bone mineral density.
6. Inflammation and Bone Health
Chronic inflammation, which is present in conditions like obesity, diabetes, and hypertension, is an important risk factor for both poor bone quality and cardiovascular disease. Inflammatory cytokines like TNF-alpha and interleukins can potentially increase the activity of osteoclasts (bone-resorbing cells) and lead to bone loss.
The presence of inflammatory markers can increase bone turnover and disrupt the balance between bone resorption and formation, leading to decreased bone mineral density (BMD) over time.
Dietary interventions such as exercise, weight loss, and anti-inflammatory diet may reduce inflammation and improve cardiovascular and bone health.
7. The Role of Exercise in Cardiometabolic and Bone Health
Physical exercise produces significant effects on cardiovascular well-being and bone density. Regular exercise, especially weight-bearing and resistance exercises, activates osteoblasts and promotes bone building, as well as reducing inflammation, improving insulin sensitivity, and improving cardiovascular health.
Aerobic exercises (e.g., walking, jogging, swimming) can help maintain cardiovascular health through improved circulation, reduced hypertension, and reduced cholesterol levels. Weight-bearing exercises like dancing, jumping, or hiking have the added benefit of improving bone density and preventing bone loss.
Strength training exercises (e.g., weight lifting) aid in maintaining muscle mass, which results in mechanical stress on bones, making the bones stronger and denser.
8. Nutritional Factors: Diet and Bone Health
Calcium and vitamin D are crucial for bone health, and a nutrient-dense diet is necessary for the maintenance of both bone density and cardiometabolic health.
Calcium is the predominant mineral in bones and maintains bone strength through adequate intake.
Vitamin D is critical for calcium absorption and bone remodeling.
Magnesium and phosphorus are also crucial in bone health.
A diet rich in fruits, vegetables, and healthy fats (such as those found in olive oil, avocados, and nuts) might suppress inflammation and promote cardiovascular and bone health.
Conversely, a high-sodium and high-sugar diet might cause both hypertension and bone loss, so the trick to maintaining peak health is balance in diet.
Conclusion
Cardiometabolic health is relevant to the maintenance of bone density and prevention of fractures and osteoporosis. All of the conditions of obesity, diabetes, hypertension, cholesterol, and inflammation contribute to bone loss and harmful cardiovascular events. Lifestyle with healthy living, physical activity, well-balanced nutrition, and tracking blood pressure, blood glucose, and cholesterol status can maximize cardiovascular and bone function.
Would you like to know more about specific strategies to improve both bone density and cardiometabolic health?
The Bone Density Solution by Shelly ManningThe program is all about healthy food and healthy habits. As we discussed earlier, we develop osteoporosis due to low bone density. Therefore, you will have to choose the right food to help your calcium and other vitamin deficiencies. In addition to healthy food, you will have to regularly practice some mild exercises. Your doctor might offer you the same suggestion. However, the difference is that The Bone Density Solution will help you with an in-depth guide.
