This eBook from Blue Heron Health NewsBack in the spring of 2008, Christian Goodman put together a group of like-minded people – natural researchers who want to help humanity gain optimum health with the help of cures that nature has provided. He gathered people who already know much about natural medicine and setup blueheronhealthnews.com. Today, Blue Heron Health News provides a variety of remedies for different kinds of illnesses. All of their remedies are natural and safe, so they can be used by anyone regardless of their health condition. Countless articles and eBooks are available on their website from Christian himself and other natural health enthusiasts, such as Julissa Clay , Shelly Manning , Jodi Knapp and Scott Davis. |
How to Identify High-Risk Individuals for Fractures
High-risk individuals for fractures need to be identified in order to take preventive action, particularly for those with a possible diagnosis of osteoporosis or other conditions that raise their risk for bone fractures. Various factors—ranging from age to lifestyle and medical history—can identify individuals at greater risk for fractures. Some important factors to be considered are as follows:
1. Age
Older individuals, especially over 65 years old, are more likely to suffer from fracture due to decreased bone density and decreased healing processes. The risk further increases with older age (generally over 80).
Women after menopause are also more likely because estrogen, which is responsible for maintaining bone strength, is lost in menopause.
Important takeaway: Postmenopausal women and the elderly are at higher risk for fracture.
2. Gender
Women, especially postmenopausal women, are at higher risk for fractures due to the loss of estrogen that affects bone health.
Men are also at risk, but bone loss typically starts later in life than in women.
Important takeaway: Women, especially postmenopausal women, are at higher risk for fractures.
3. Previous Fractures
Individuals with a history of previous fractures, especially after minor falls or injuries, are also at higher risk of subsequent fractures. The bone strength of individuals who have previously fractured a bone may be compromised and lead to subsequent fractures.
Key takeaway: History of fracture increases the risk of future fractures.
4. Bone Mineral Density (BMD)
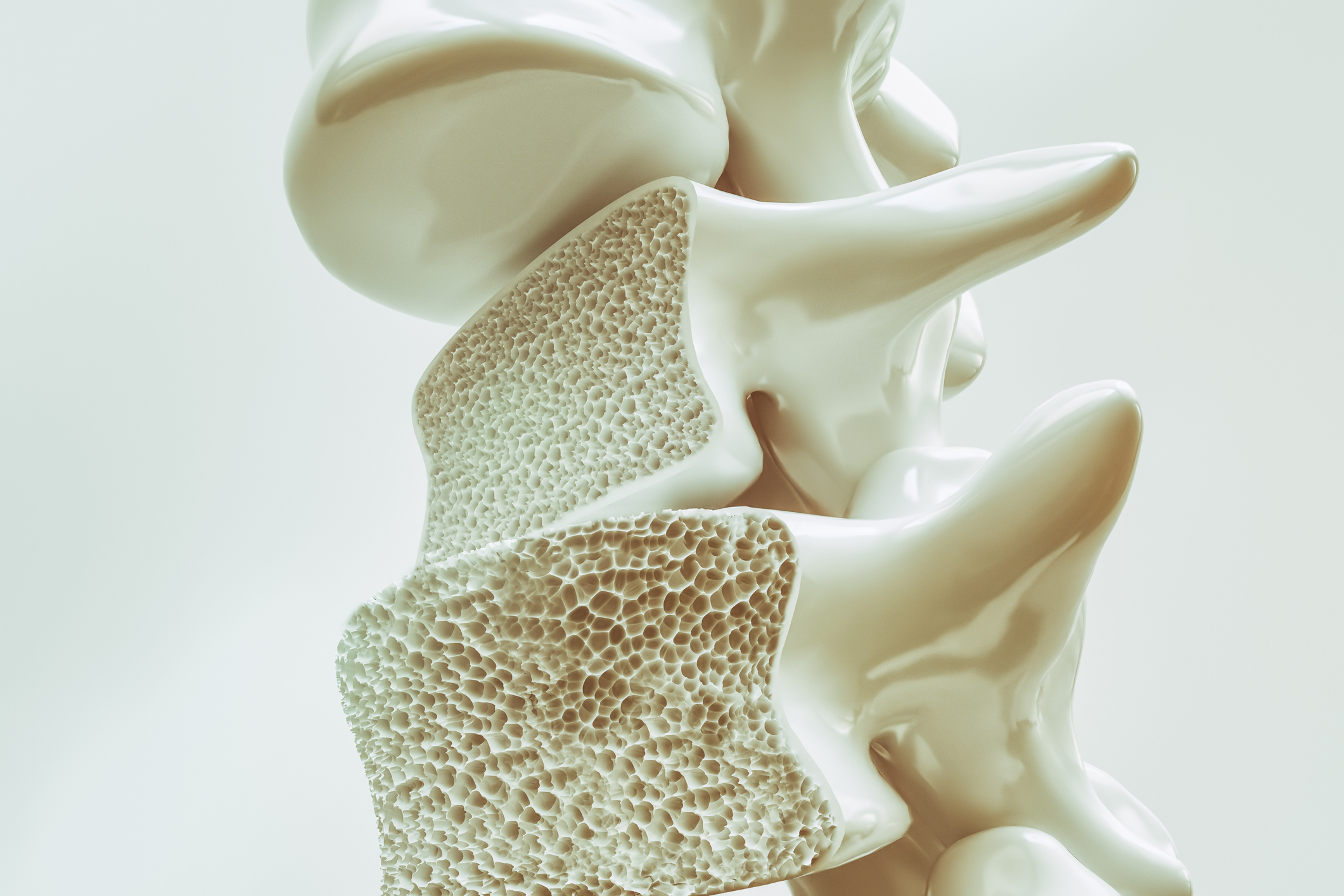
Low bone mineral density (BMD) is perhaps the most significant osteoporosis marker and strongest predictor of fracture risk. BMD testing, typically done with a DEXA scan, measures bone density and identifies individuals at risk.
The lower the BMD, the higher the risk for fracture, especially in the spine, hip, and wrist.
Key point: Low bone mineral density (as measured by a DEXA scan) is a strong risk factor for fractures.
5. Chronic Medical Conditions
The most common condition with increased risk of fracture is osteoporosis. Osteoporosis patients have compromised bones and are more likely to suffer from fractures.
Chronic disease, like rheumatoid arthritis, diabetes, and renal disease, contributes to fracture risk since these diseases are associated with bone metabolism, balance, and muscle strength disturbances.
Hypothyroidism and disorders in calcium metabolism (e.g., hyperparathyroidism) also increase the risk of fracture.
Most important take away: Fracture risk is increased with chronic disease, especially osteoporosis.
6. Drugs
Certain medications compromise bone health to the point of elevating the risk of fracture. Examples of such drugs include:
Corticosteroids (like prednisone), which reduce bone density over the long term.
Anti-seizure medications, diuretics, and some chemotherapy.
Proton pump inhibitors (PPIs) that influence calcium absorption.
Antidepressant and antipsychotic medications, which impair balance and coordination, making people more prone to falls.
Key point: Taking some drugs for an extended period of time can result in brittle bones and higher fracture risk.
7. Low Body Weight and Poor Nutrition
Individuals who have low body weight or malnutrition, particularly those with an insufficiency of calcium and vitamin D, are at a higher risk for fractures. Strength of bones relies on adequate nutrients, and malnutrition can inhibit bone repair and formation.
Eating disorders like anorexia nervosa may also increase the risk of fracture through inadequate bone mineralization.
Malnutrition, especially deficiency in calcium and vitamin D, and low body weight are the factors of increased risk of fracture.
8. Family History of Osteoporosis or Fractures
Family history of osteoporosis or fractures increases the risk for a person to develop the same issues. Heredity is a factor in bone structure and density.
Important takeaway: Family history of fractures or osteoporosis may increase individual fracture risk.
9. Lifestyle Factors
Physical inactivity and a sedentary lifestyle increase the risk of fractures through contributing to muscle weakness, impaired balance, and reduced bone strength.
Bone loss and poor body fracture healing abilities are triggered by smoking and excessive alcohol consumption.
Physical inactivity, particularly weight-bearing activity, reduces bone strength and heightens the danger of fractures.
Key point to recall: Risk of fractures increases with inactivity, smoking, and excessive alcohol consumption.
10. Balance and Fall Risk
Poor balance, vision loss, and inability to perform daily activities safely increase the risk of falls, which can lead to fractures. Dizziness, neuropathy, and muscle weakness (typically due to aging or disease) are significant contributors.
Important takeaway: Poor balance and vision loss increase the risk of falls, which can lead to fractures.
11. Ethnicity
Certain ethnic groups will have a higher or lower risk of fractures. Caucasians and Asians, for instance, have a higher risk of osteoporosis and fractures compared to Black and Hispanic groups.
Key point: Ethnicity may have an effect on fracture risk, with certain groups being more at risk because of differences in bone density and health.
12. Menopause and Hormonal Changes
Decline in estrogen during menopause causes increased loss of bone, and women post-menopause are very prone to fractures. Estrogen maintains the bones, and decline in estrogen causes a decline in bone mineral density, hence the predisposition to fractures.
Key takeaway: Menopause and loss of estrogen increase fracture risk in women.
Screening for High-Risk Patients
To screen high-risk patients for fractures, the following tools and tests are utilized by physicians:
Fracture risk estimates such as the FRAX tool (calculation of fracture risk using clinical parameters).
Measurement of bone mineral density (DEXA scan).
Physical examination to evaluate balance, strength, and mobility.
Conclusion:
Selection of high-risk fracture individuals involves consideration of a combination of age, medical history, medications, life style, and family history. Early identification permits preventive measures such as bone densitometry for screening, supplementations with calcium and vitamin D, exercise, and some medicines to reduce fracture risk. Effective screening and prevention can make significant contributions to decreasing the impact of fractures, particularly in high-risk populations.
Bone density monitoring is a significant tool for the prevention of fractures, particularly in individuals who are at risk for osteoporosis and other bone diseases. Through the monitoring of bone mineral density (BMD), one can assess the strength of bones and risk for fracture, and in addition to this, have the ability to intervene early enough to stop the fracture. Below is an analytical discussion on how bone density monitoring prevents fractures.
1. Osteoporosis Early Detection
Bone mass measurement, commonly by a DEXA (dual-energy X-ray absorptiometry) scan, can detect osteoporosis and low bone mass at an early point, often before a fracture occurs. Osteoporosis is a medical condition in which bones become weak and brittle such that they easily break, often in the spine, hip, and wrist.
Early identification of low bone density allows early treatment to strengthen bones and reduce the risk of fractures, often by modifying lifestyle, medication, and other treatments.
Key point: Early measurement of bone density detects low bone mass or osteoporosis early, allowing for immediate treatment and prevention of fractures.
2. Fracture Risk Assessment
The BMD score can also be used to measure fracture risk. Low BMD (typically a T-score of -2.5 or worse) is an excellent predictor of increased fracture risk. Regular bone density testing provides information on how fast bone density is decreasing and whether the individual is at greater risk for fractures.
The FRAX algorithm, including BMD along with other clinical factors (age, gender, smoking, and history of fractures), is also helpful in estimating the risk of major fractures, i.e., hip, spine, and wrist fractures.
Important point: Bone density screening plays a crucial role in fracture risk prediction as well as in deciding whether to give or not give preventive treatments.
3. Guiding Treatment Decisions
Monitoring bone density over a period of time enables doctors to tailor treatments in accordance with an individual’s fracture risk. For example, low BMD patients can be administered bisphosphonates, denosumab, or teriparatide that halt bone loss and reduce fractures.
Bone density testing also helps to alter treatments whenever bone density goes up or down, so the patient receives optimal treatment.
Key takeaway: Routine bone density testing guides treatment choices to avoid continued bone loss and fractures.
4. Assessing the Effectiveness of Interventions
For those who are already under treatment for osteoporosis or other bone disorders, bone density tests can be employed to quantify the effectiveness of the treatment. When the treatment is effective, bone density stabilizes or increases minimally. If bone density keeps declining, the treatment regimen might have to be modified.
Monitoring also helps to track changes in bone health after lifestyle modifications, such as increased physical activity, diet, or supplements like calcium and vitamin D.
Important takeaway: Bone density monitoring helps to evaluate the effectiveness of treatments and lifestyle modifications in preventing fractures.
5. Identifying Individuals at High Risk
Certain groups are more vulnerable to fractures according to age, gender, family history, and medical conditions. Bone densitometry is particularly important for individuals who have:
Postmenopausal women due to the deprivation of estrogen, which aids in bone loss.
Older persons who naturally lose bone density with advancing age.
Individuals who have had fractures, have a family history of osteoporosis, or chronic conditions (e.g., rheumatoid arthritis, diabetes, or kidney disease) that increase the risk of fractures.
Bone density tests detect these individuals so that preventive interventions are begun early.
Key takeaway: Bone density monitoring is especially important in high-risk groups, allowing early intervention and prevention of fractures.
6. Preventing Hip and Vertebral Fractures
The most disabling fracture forms are hip and vertebral fractures, which normally lead to loss of mobility, persistent pain, and decreased quality of life. Through the identification of low bone density by monitoring, targeted prevention (e.g., drugs, fall prevention measures, or exercise regimens) can significantly reduce the risk of such disabling fractures.
Silent vertebral fractures may occur without any overt symptoms, and as such routine bone density measurements can detect them before they result in chronic back pain or deformity.
Point to remember: Bone density screening avoids disabling and severe fractures of the hip and vertebrae.
7. Incorporating Bone Health into Overall Care
Bone density screening must be made as part of a holistic health approach, especially in individuals over 50 years or those with osteoporosis risk factors. Along with BMD screening, patients must be given comprehensive care such as:
Dietary advice, with an emphasis on calcium and vitamin D-rich foods.
Physical therapy advice, like weight-bearing exercises to build bones and balance.
Prevention from falls, especially among old or balance-impaired individuals.
Key take-home: Measurement of bone density is a part of an overall plan with diet, exercise, and avoidance of falls in preventing fractures.
8. Surveillance of Change in Bone Status
For those with an intermediate risk of fractures, serial bone density tests might be prescribed every 1-2 years to track changes in bone density over time. This way, professionals can identify any reason for concern early and implement changes to treatment to prevent fractures.
Tracking in this manner ensures that individuals who do not yet have osteoporosis or fractures are nevertheless protected before the loss of bones is severe.
Top note: Regular monitoring of bone density follows what occurs over the years and prevents fractures before they happen.
Conclusion
Bone density monitoring is important in fracture prevention, especially in individuals at high risk. Regular monitoring with DEXA scans and the use of risk assessment instruments like FRAX help detect early osteoporosis, assess fracture risk, guide treatment, and measure intervention effectiveness. With early detection, lifestyle changes, and correct medical treatments, one can maintain bone health and avoid fractures as they grow old.
The Bone Density Solution by Shelly ManningThe program is all about healthy food and healthy habits. As we discussed earlier, we develop osteoporosis due to low bone density. Therefore, you will have to choose the right food to help your calcium and other vitamin deficiencies. In addition to healthy food, you will have to regularly practice some mild exercises. Your doctor might offer you the same suggestion. However, the difference is that The Bone Density Solution will help you with an in-depth guide.
